Data Points | When COVID-19 Meets Structural Inequity, Chicago’s Immigrant Population Suffers

COVID-19 has raised questions about the underlying reasons why immigrants are being disproportionately impacted by the crisis. Racism and a legacy of unfair policies permeate immigrants’ lives, with devastating community outcomes. In this two-part Data Points series, MPC explores some structural and economic barriers that leave our immigrant community vulnerable to Coronavirus.
Navigating America’s health care system is difficult for everyone on a good day. It’s worse in a pandemic. And for people with limited English skills and access to healthcare, the problems compound.

Earlier this spring, Chicago saw a dramatic rise in COVID-19 cases among its immigrant community, particularly in zip codes with a high number of immigrant residents, motivating the MPC Data Team to investigate: Why is this population among the hardest hit by the pandemic? In Part One of this special two-part Data Points series, we examined how immigrants’ housing and employment conditions and their legal status may relate to COVID-19 vulnerabilities. But that is only part of the story. Now in Part Two we look how additional structural barriers, such as limited access to health care, potentially exacerbate the impact of COVID-19 among immigrant populations.
Immigrants’ Access to Health Care: One of every four immigrants living in Chicago lack health insurance
Immigrants face several challenges in accessing health care. They are more likely to work in insecure, low-paid jobs that either make it difficult to afford health insurance or don’t offer employer-based coverage. Additionally, barriers such as high coverage costs, fear of deportation, stricter eligibility requirements/lack of legal status, little knowledge about how to navigate the system, administrative burdens, and language prevent many immigrants from accessing health care services.
The uninsured rate for non-U.S. citizens is almost four times higher than that of naturalized citizens.
Immigration policies, particularly under the Trump administration, have also discouraged immigrants from seeking health care. With the public charge rule, a rule that ties legal status and citizenship to not utilizing public benefits, many are afraid of accepting any kind of public benefits because that could impact their chances of obtaining legal citizenship. Undocumented immigrants are at a disadvantage since they do not qualify for health coverage benefits, and those with U.S.-citizen children may not realize that their children are eligible or may be reluctant to enroll them for fear their legal status becomes known.
As the Coronavirus continues to spread, these and additional barriers impede an effective response to the pandemic, leading immigrants, even eligible ones, to take insurance and other benefits at lower rates that U.S.-born citizens. Avoiding care during the pandemic or delaying treatment could risk immigrants’ and their broader communities’ health.
As shown in Figure 1, the uninsured rates of the Chicago immigrant population are higher than the rates of the native-born population. Overall, 24.9% of immigrants living in Chicago lack health insurance coverage compared to 7% of native-born Americans. Among immigrants, citizenship status influences their likelihood of having health coverage. The uninsured rate for non-U.S. citizens is almost four times higher than that of naturalized citizens.
Figure 1. Chicago Uninsured Rates by Citizenship Status, 2018: The health insurance gap for immigrants is very high in Chicago
COVID-19 is not impacting the city evenly. Communities where Latinx and minority residents are concentrated have become major hotspots. This is the case of the South and West Sides, whose residents, long affected by income and housing insecurity, are also less likely to have health insurance coverage. As the map in Figure 2 shows, a high concentration of uninsured immigrants also live in many of these areas.
Figure 2. COVID-19 cases are high in most communities with a high percentage of immigrants without health insurance
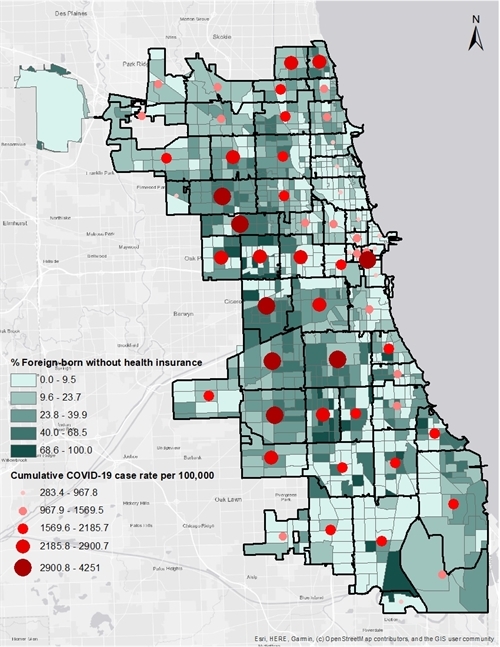
Data Source: U.S. Census Bureau, 2014-2018 American Community Survey 5-Year Estimates; City of Chicago Data Portal: COVID-19 Cases, Tests, and Deaths by Zip Code dataset (as of July 18, 2020)
The map in Figure 3 shows that workers most likely to enjoy employer-based health insurance are concentrated in Chicago’s affluent neighborhoods. This distinct neighborhood-level impact is a reflection of Chicago’s history of racial and economic segregation. It is not surprising that COVID-19 has a small impact on more affluent areas while disproportionately affecting majority-minority neighborhoods.
Figure 3. COVID-19 cases tend to be lower among communities with employer-based health insurance
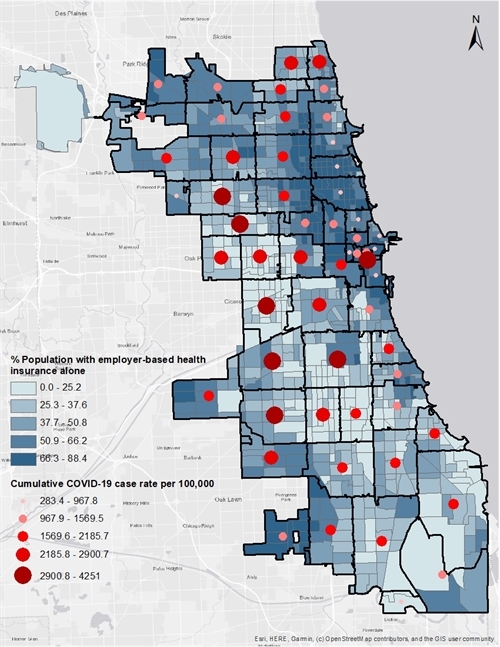
Data Source: U.S. Census Bureau, 2014-2018 American Community Survey 5-Year Estimates; City of Chicago Data Portal: COVID-19 Cases, Tests, and Deaths by Zip Code dataset (as of July 18, 2020)
Language Barriers. Language barriers not only limit people’s access to health and human services programs but also reduce their access to public information about prevention, treatment, recovery, and other aspects of COVID-19. These barriers can islolate limited English speakers, leaving them without proper information and care, putting them at greater risk of suffering from the Coronavirus crisis.
As the Coronavirus spreads across the country, the Federal government and some industries have been criticized for failing to provide timely translations of Coronavirus-related information, leaving limited English speakers isolated from the news.
Almost 15% of the Chicago population speak English “less than very well,” but this figure is higher among the immigrant population. In 2018, Chicago was home to 558,874 immigrant residents, and about 56.5% of them self-reported speaking English “less than very well.” Whether that means they don’t speak a word or understand half of what they hear, they struggle to some degree with language barriers.
Keeping up to date about the Coronavirus can be a problem for individuals with limited English language skills. Public information about COVID-19 is not as frequently distributed and updated in languages other than English. As the disease spreads across the country, the Federal government and some industries have been criticized for failing to provide timely translations of Coronavirus-related information, leaving limited English speakers isolated from the news. This is particularly crucial during the pandemic, given that information is changing rapidly as health experts learn more about the virus.
Language barriers may limit an individual’s ability to seek health care, thus delaying early intervention and tracking of COVID-19. Research shows that individuals whose main spoken language is not English are less likely to understand the processes necessary to become insured and to remain insured, to receive preventative care, to have a regular source of primary care, and to receive timely physical examinations. Language barriers may also cause misdiagnosis and limit the understanding of guidelines and recommendations for treatment and follow-up visits.
The significant number in COVID-19 cases among Chicago immigrant communities suggests that health experts and elected official are failing to reach out to limited English speakers before the virus spreads among them.
Figure 4. Percentage of Limited English Speakers in Chicago by Citizenship Status, 2018: Language is a barrier for half to two-thirds of immigrant populations
This outbreak raises questions about working and living conditions, job security, and lack of accountability in the current immigration system. While in Part One of this Data Points series, we explored how the risk of transmission is particularly high in certain industries and living conditions, iit is clear that the risk of getting sick is also being exacerbated during the pandemic by language barriers and limited access to health care.
The COVID-19 crisis makes clear that it is time for an effective policy response that not only tackles consequences but also addresses the underlying reasons some communities are disproportionately impacted by COVID-19. Racism and a legacy of unfair immigration policies that reinforce discrimination are inextricably linked to the overall health of the immigrant community. The data reveal that systematic discrimination and exclusion have contributed to stark and persistent disparities in the well-being of immigrants, especially between those who have become U.S. citizens and those who remain non-U.S. citizens.
Federal responses should acknowledge the diversity of the population not only due to gender, income, education, religion, age, but also their legal status and language. Overcoming these barriers not only will require reforms of the government institutions and the provision of government services, but also for employers to alter their sick leave policies. Immigrant workers need not choose between job security and their health. Policies should protect all immigrants, regardless of legal status, and ensure they are in a better position to take care of themselves and contribute to their communities.
We can no longer ignore the barriers of discrimination and structural racism that exist in our society, which contribute to immigrants being more likely to suffer from poverty and work in insecure, low-paid jobs. The rise in COVID-19 cases has raised alarms about equity issues facing immigrants. Once the crisis is over, we need a new social contract that advances causes of racial and economic equality.